Introduction
The urease test is a biochemical test used to detect the presence of urease enzymes in bacterial cells or clinical specimens. The test involves adding a sample of the bacterial culture or clinical specimen to a medium containing urea and a pH indicator. If the bacteria produce urease, the enzyme will hydrolyze urea, releasing ammonia and increasing the pH of the medium. The pH indicator will change color from yellow to pink, indicating a positive result for urease activity.
Importance of the urease test in bacteriology
The urease test is an important diagnostic tool in bacteriology, as it can be used to identify bacterial species that produce urease and diagnose infections caused by these bacteria. Urease-positive bacteria are important in medical microbiology, as they are often responsible for urinary tract infections, gastritis, and other medical conditions.
Identification of bacterial species
The urease test can be used to identify bacterial species that produce urease. For example, Helicobacter pylori is a bacterial species that is responsible for peptic ulcers and gastritis. This bacterium produces urease, which helps it survive in the acidic environment of the stomach. The urease test can be used to confirm the presence of H. pylori in clinical specimens.
Diagnosis of infections
The urease test can also be used to diagnose infections caused by urease-positive bacteria. For example, Proteus mirabilis is a common cause of urinary tract infections. This bacterium produces urease, which can cause the urine pH to become alkaline and promote the formation of kidney stones. The urease test can be used to diagnose P. mirabilis infections by detecting the presence of urease in the urine.
Principle of Urease Test
The urease test is based on the ability of certain bacteria to produce the enzyme urease, which converts urea to ammonia and carbon dioxide. This enzymatic reaction is used as the basis of the urease test. The principle of the urease test can be summarized as follows:

Urease Production:
The first step in the urease test is to determine whether the bacteria being tested are capable of producing the enzyme urease. Urease-positive bacteria are capable of hydrolyzing urea, a compound found in many culture media, into ammonia and carbon dioxide. Urease-negative bacteria, on the other hand, are unable to produce this enzyme.
Hydrolysis of Urea:
The second step in the urease test involves the hydrolysis of urea. In the presence of urease, urea is converted into ammonia and carbon dioxide. This reaction causes an increase in pH, which can be detected using a pH indicator. The pH indicator changes color from yellow to pink as the pH increases, indicating the presence of urease.
Detection of Urease:
The third step in the urease test is to detect the presence of urease. This is done by adding a sample of the bacterial culture or clinical specimen to a medium containing urea and a pH indicator. If the bacteria produce urease, the enzyme will hydrolyze urea, releasing ammonia and increasing the pH of the medium. The pH indicator will change color from yellow to pink, indicating a positive result for urease activity.
Rapid Urease Test
The rapid urease test is a diagnostic test used to detect the presence of the bacterium Helicobacter pylori in the stomach. The test is based on the ability of H. pylori to produce urease, an enzyme that catalyzes the hydrolysis of urea into ammonia and carbon dioxide. The test involves taking a biopsy sample of the stomach lining and placing it on a special test strip that contains urea and a pH indicator. If H. pylori is present in the biopsy sample, it will produce urease, leading to an increase in pH that is detected by the pH indicator. The test can provide results in as little as 30 minutes and is considered highly accurate.
Urea Breath Test:
The urea breath test is another diagnostic test used to detect the presence of H. pylori in the stomach. The test involves giving the patient a drink containing a small amount of radioactive carbon-13-labeled urea. If H. pylori is present in the stomach, it will produce urease, leading to the hydrolysis of the labeled urea into carbon dioxide and ammonia. The patient then breathes into a special bag, and the level of radioactive carbon dioxide in the breath is measured using a special machine. If the level of radioactive carbon dioxide is high, it indicates the presence of H. pylori in the stomach. The test is non-invasive, does not require a biopsy, and can provide results within 30 minutes.
Media Used in Urease Test
The urease test is a biochemical test that detects the presence of urease activity in bacterial species. The test is based on the hydrolysis of urea by urease enzyme, resulting in the production of ammonia and carbon dioxide. Several media are available for performing the urease test, including:
Christensen’s urea agar
Christensen’s urea agar is a commonly used medium for the urease test. It contains peptone, beef extract, and urea as the main ingredients. Phenol red is used as an indicator that changes color from yellow to pink when the urea is hydrolyzed to ammonia by the bacterial urease.
Stuart’s urea broth
Stuart’s urea broth is a liquid medium that contains urea, peptone, and other nutrients. Phenol red is used as an indicator that changes color from yellow to pink when the urea is hydrolyzed to ammonia by the bacterial urease. Stuart’s urea broth is a useful medium for the detection of urease activity in fastidious bacterial species that do not grow well on solid media.

Urease agar
Urease agar is a solid medium that contains yeast extract, peptone, and urea. It also contains a pH indicator such as phenol red or bromothymol blue that changes color from yellow to pink or blue when the urea is hydrolyzed to ammonia by the bacterial urease.
Materials required for the test
- Urease test medium (e.g., Christensen’s urea agar, Stuart’s urease medium, etc.)
- Sterile loop or wire
- Inoculating needle or loop
- pH indicator (e.g., phenol red, bromocresol purple, etc.)
- Sterile distilled water
- A bacterial culture or clinical specimen
Procedure for performing the urease test
- Using a sterile loop or wire, inoculate the urease test medium with the bacterial culture or clinical specimen being tested.
- Incubate the inoculated medium at the appropriate temperature and for the appropriate time period required for the specific bacterial species being tested.
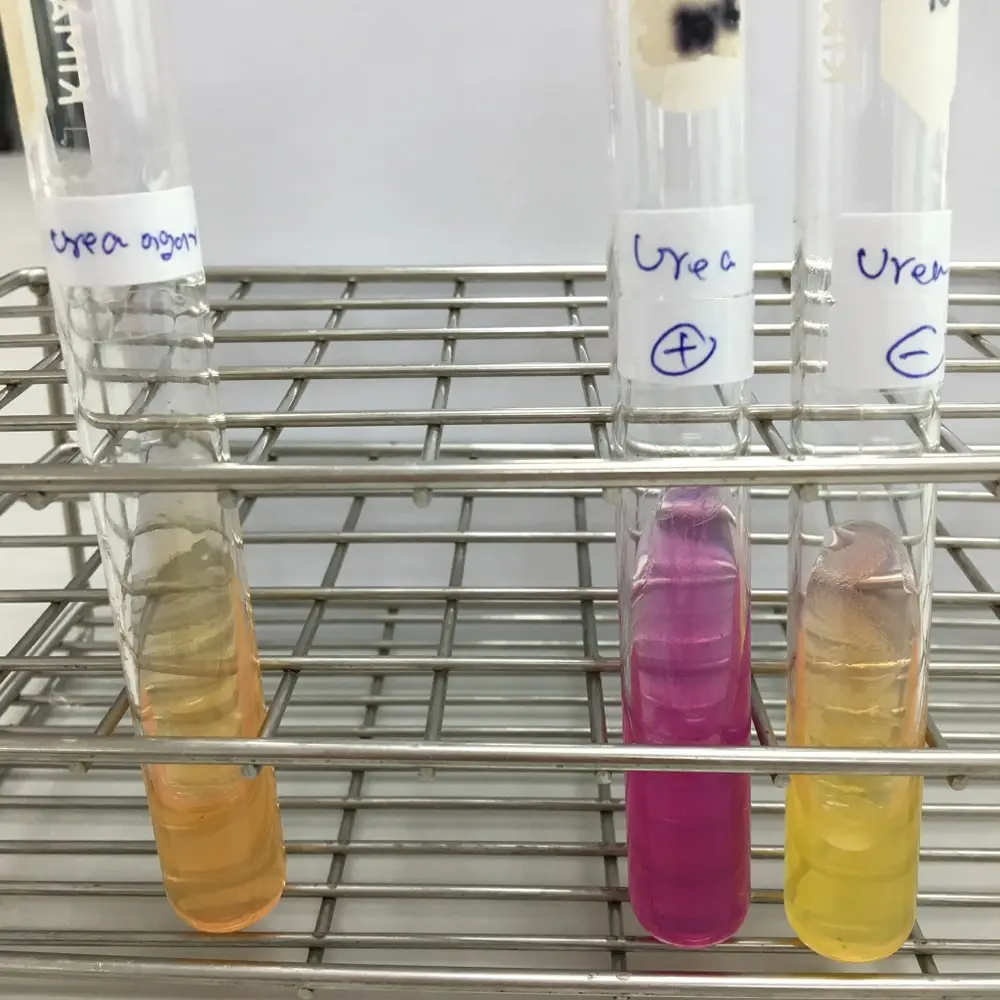
- After incubation, observe the medium for a change in pH. The pH indicator in the medium will change color from yellow to pink if the bacteria produce urease, indicating a positive result for urease activity. A negative result is indicated by no change in the color of the pH indicator.
Interpretation of results
Interpretation of the results of the urease test involves the following:
Positive Result: A positive result for urease activity is indicated by a change in the color of the pH indicator from yellow to pink. This indicates that the bacteria being tested are capable of producing urease.
Negative Result: A negative result is indicated by no change in the color of the pH indicator. This indicates that the bacteria being tested are not capable of producing urease.
Quality control measures
To ensure the accuracy and reliability of the urease test, the following quality control measures should be taken:
- Positive and negative controls should be included in each test run to ensure that the test is working correctly.
- The urease test medium should be prepared according to the manufacturer’s instructions and stored properly.
- Sterile techniques should be followed when inoculating the medium to avoid contamination
- The incubation time and temperature should be standardized for the specific bacterial species being tested.
Significance of Urease-Positive Bacteria
Urease-positive bacteria are bacterial species that are capable of producing the enzyme urease, which hydrolyzes urea to ammonia and carbon dioxide. The significance of urease-positive bacteria lies in their physiological and pathological consequences.
Types of bacteria that produce urease:
Urease production is a common trait among many bacterial species. Some of the most common urease-positive bacteria include Proteus, Klebsiella, Pseudomonas, Helicobacter pylori, and Corynebacterium urealyticum. Urease production is also seen in some fungal species, such as Candida albicans.
Physiological significance of urease production:
Urease production by bacteria has several physiological functions. Urea is a nitrogen-containing compound that is produced during protein metabolism in animals. Urease-positive bacteria can use urea as a nitrogen source and as a way to buffer the pH of their environment. Urease production can also enhance bacterial motility by increasing the pH gradient between the inside and outside of the bacterial cell.
Pathological consequences of urease production:
The pathological consequences of urease production by bacteria can be significant. Urease-positive bacteria can cause urinary tract infections, as the production of ammonia by these bacteria can lead to the formation of alkaline urine and the precipitation of minerals, such as calcium, leading to the formation of urinary stones. Urease-positive bacteria can also cause infections in other parts of the body, such as the respiratory and gastrointestinal tracts.
Helicobacter pylori, a urease-positive bacterium, is associated with the development of peptic ulcers and gastric cancer. The production of urease by H. pylori enables it to survive in the acidic environment of the stomach by neutralizing the acid and creating a more hospitable environment. This, in turn, can lead to chronic inflammation and damage to the gastric mucosa.
Clinical Applications of the Urease Test
The urease test has several clinical applications in the diagnosis and treatment of various bacterial infections. Some of the clinical applications of the urease test include:
Diagnosis of Helicobacter pylori infections
The urease test is a useful diagnostic tool for detecting the presence of Helicobacter pylori, a bacterium that causes chronic gastritis, peptic ulcer disease, and gastric cancer. The urease test is performed on biopsy specimens collected during an endoscopy procedure. The biopsy specimen is placed in a medium containing urea and an indicator that changes color when the urea is hydrolyzed to ammonia by H. pylori urease. The color change indicates the presence of H. pylori in the biopsy specimen.
Detection of Proteus mirabilis in urinary tract infections
Proteus mirabilis is a urease-positive bacterium that is commonly associated with urinary tract infections (UTIs). The presence of P. mirabilis in the urine can cause alkaline urine, which can lead to the formation of urinary stones. The urease test can be used to detect the presence of P. mirabilis in urine specimens. The test is performed by adding a urea-containing reagent to the urine sample and observing for the production of ammonia, which is indicated by a color change in the medium.
Identification of other urease-positive bacterial species
The urease test can also be used to identify other urease-positive bacterial species, such as Klebsiella, Pseudomonas, and Corynebacterium urealyticum, which are associated with various infections. The test is performed by inoculating the bacterial culture onto a medium containing urea and an indicator that changes color when the urea is hydrolyzed to ammonia by the bacterial urease. The color change indicates the presence of urease-positive bacteria in the culture.
Limitations and Drawbacks of the Urease Test
The urease test is a widely used diagnostic tool in bacteriology; however, it has some limitations and drawbacks that should be considered when interpreting test results. Some of the limitations and drawbacks of the urease test include:
False-positive results due to contamination
The urease test is prone to false-positive results due to contamination of the test medium with urease-producing microorganisms. Contamination can occur during sample collection, processing, or handling, leading to inaccurate test results. It is important to perform proper aseptic techniques during sample collection and processing to minimize the risk of contamination.
False-negative results due to low bacterial load
The sensitivity of the urease test depends on the bacterial load present in the sample. Low bacterial loads may result in false-negative results, where the test fails to detect the presence of urease-producing bacteria. False-negative results can occur in early stages of infection or in cases where the bacterial load is low.
Interference from acidic or alkaline pH
The accuracy of the urease test can be affected by the pH of the test medium. Acidic or alkaline pH can interfere with the activity of urease, leading to inaccurate test results. It is important to maintain a proper pH range for the test medium to ensure accurate results.
References
- Tortora, G. J., Funke, B. R., & Case, C. L. (2021). Microbiology: An introduction. Pearson Education Limited.
- Willey, J. M., Sandman, K. M., Wood, D. H., & Prescott, L. M. (2019). Prescott’s microbiology (11th ed.). McGraw Hill.
- Cappuccino J.G. and Sherman N. 2008. Microbiology: A Laboratory Manual, 8th ed. Pearson Benjamin Cummings, San Francisco, CA, USA.
- https://asm.org/Protocols/Urease-Test