Introduction:
Opsonization functions in our immune system like a superhero, controlling behind the scenes to keep us healthy. Imagine it as a protective barrier with small soldiers known as antibodies and complement proteins working together to label bad guys (pathogens) for capture.
These little warriors ensure that our cleanup team, the phagocytes, know whom exactly to target. It’s like a well-choreographed dance in which immune cells and antibodies work together to attack the invaders. Opsonization isn’t just a unique term; it’s the immune system’s way of displaying its abilities while keeping us safe from challenging germs.
Opsonization Definition:
Opsonization, derived from the Greek word “opsono,” which means “prepare a feast,” is an important immunological process in which foreign particles, such as bacteria or viruses, are chosen for destruction by the immune system. This preparation requires coating these pathogens with opsonins, which are chemicals that boost immune cell identification and phagocytosis (engulfing and digesting).
Key players in opsonization:
Several major players take part in the challenging dance of opsonization, each playing an important role in this defense mechanism. These key players are:
- Antibodies
- Complement proteins
- Phagocytes (macrophages and neutrophiles)
Antibodies or immunoglobulins
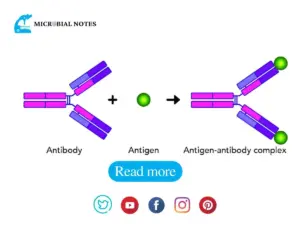
Assume antibodies to be the opsonization’s superheroes. These Y-shaped proteins, which are produced by B cells, have specialized locations that lock onto antigens, which are pathogen-specific indicators. Antibodies identify invaders by attaching to these antigens, making them obvious targets for the immune system.
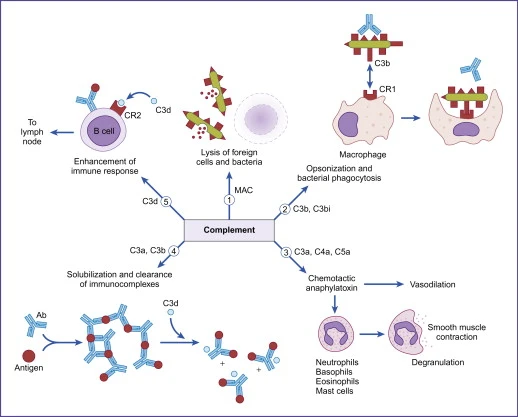
Complement proteins:
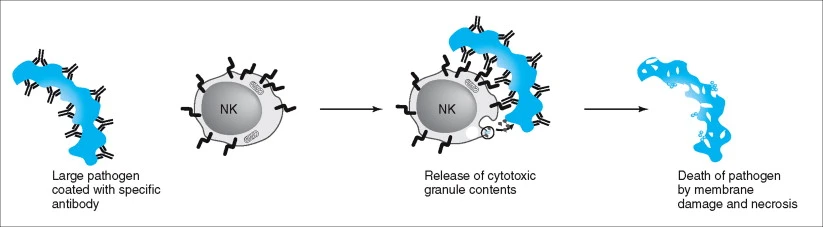
Look at complement proteins to be the partners that aid antibodies. They can directly bind to pathogens or collaborate with antibodies to generate strong complexes. When the complement system is activated, membrane attack complexes are formed, which create cracks in the invaders, weakening them for capture.
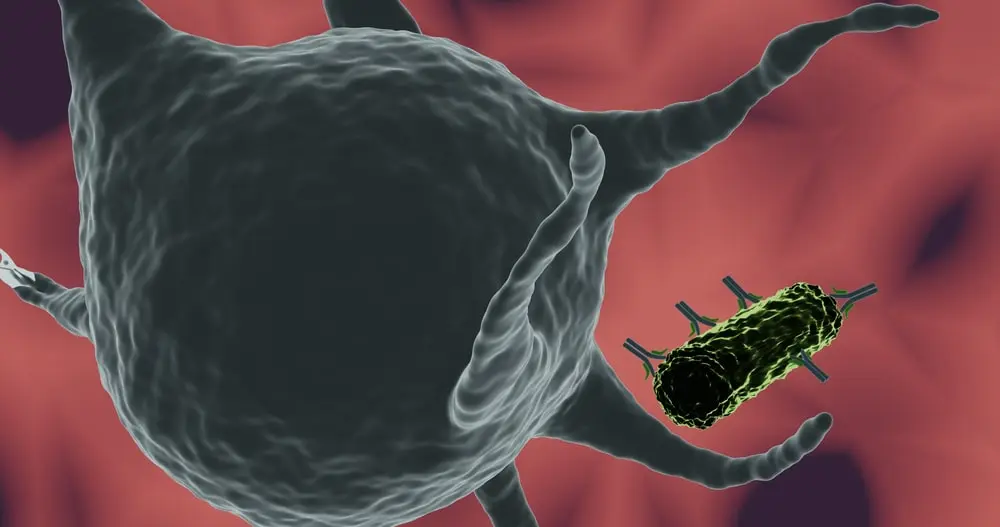
Phagocytes (macrophages and neutrophils)
Phagocytes are the cleanup team, ready to engulf and digest the identified invaders. These immune cells, which are equipped with receptors that recognize opsonins, efficiently identify and digest pathogens. It’s like a superhero team-up: antibodies and complement proteins identify the evil guys, and phagocytes rush in for the murder.
Mechanism of Opsonization:
Opsonization is a complicated immunological response that includes antibodies, complement proteins, and phagocytosis. This process improves pathogen detection and clearance by phagocytic cells. Here’s an in-depth discussion of the opsonization process, which includes antibodies, complement proteins, and phagocytosis:
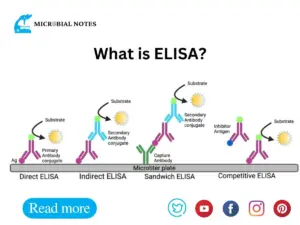
1. Antibody-Mediated Opsonization
Antibody-mediated opsonization is a type of immunological response that involves antibodies attaching to pathogens and labeling them for detection and phagocytosis by immune cells. This mechanism plays an essential role in the effective removal of infections from the body. Here’s a further in-depth explanation of antibody-mediated opsonization:
Antigen recognition and Antibody production
- When an infectious agent enters the body, B cell lymphocytes recognize antigens that are on its surface.
- Activated B cells develop into plasma cells, which produce antibodies (immunoglobulins), particularly IgG and IgM.
Antigen-Antibody binding
- Antibodies attach to antigens on pathogen surfaces via antigen-binding sites that exist within antibody molecules’ Fab (Fragment, antigen-binding) regions.
- The variable sections of the Fab regions determine the specificity of antibody binding, allowing antibodies to recognize and attach to specific epitopes on the pathogen.
Opsonin exposure
- Following antigen-antibody interaction, the Fc region of the antibody (Fragment, crystallizable) is revealed. This area is not involved in antigen binding but is critical for interactions with other immune system components.
Recognition by phagocytes
- Fc receptors on the surfaces of phagocytic cells, such as macrophages and neutrophils, recognize and bind to the Fc portion of antibodies.
- This binding improves the phagocyte’s interaction with the opsonized pathogen.
Phagocytosis Initiation
- Fc receptor activation activates intracellular signaling pathways within the phagocyte.
- These signaling events activate systems that enhance phagocytosis.
Pseudopodia Extension and Phagosome Formation
- The phagocyte forms a phagosome by extending pseudopodia to engulf the opsonized pathogen.
- Opsonins, which include antibodies, cover the pathogen inside the phagosome.
Fusion with Lysosomes
The phagosome that contains the opsonized pathogen joins forces with lysosomes, which are organelles that contain enzymes and other antimicrobial chemicals.
Pathogen Destruction
- Internalized pathogens are degraded by lysosomal enzymes such as proteases and lysozymes.
- Within the lysosomes, reactive oxygen species (ROS) and other antimicrobial chemicals help to destroy the pathogen.
Exocytosis of Residual Material
- Exocytosis is the process by which pathogen leftovers, now broken down into tiny particles, are discharged from the phagocyte.
Resolution of Inflammation
- Once the pathogen has been eliminated, the immune response modulates inflammation to prevent excessive tissue damage.
In short, antibody-mediated opsonization involves antibodies attaching to pathogens, which improves their detection by phagocytes via Fc receptors. This process facilitates efficient phagocytosis and subsequent pathogen elimination, contributing to total immunological defense against infections.
Complement-Mediated Opsonization
Complement-mediated opsonization is an important phase in the immune system that dramatically improves phagocytic cells’ ability to find, bind to, and remove pathogens. This complicated system functions as a key component of the innate immune response, aiding the body’s defense against a variety of pathogenic pathogens.
The Complement System: A Complex Cascade
The complement system, a complex network of proteins, is essential in the innate immune response. It is made up of three key activation pathways: classical, lectin, and alternative, all of which work together to stimulate the synthesis of C3 convertase.
Activation Pathways
- Classical pathway: Immune complexes and antibody binding initiate the classical pathway.
- Lectin Pathway: This pathway is activated when lectin binds to microbial surfaces.
- Alternative Pathway: Started by C3 spontaneous hydrolysis.
Formation of C3 Convertase
Activation of any pathway results in the production of C3 convertase, an enzyme complex that cleaves C3 into its active components, C3a and C3b.
Role of C3b in Opsonization
C3b, a key component in complement-mediated opsonization, attaches covalently to pathogen surfaces, marking them for detection and destruction by phagocytic cells.
Mechanism of Complement-Mediated Opsonization
- C3 Convertase Facilitation: The production of C3 convertase following complement activation facilitates the process.
- C3b functions as an opsonin, improving phagocytic detection of infections.
Receptor-Mediated Recognition
Phagocytic cells, such as macrophages and neutrophils, express particular receptors, such as CR1 and CR3, that recognize and bind to C3b-coated pathogens, triggering phagocytosis.
Enhancement of Phagocytosis
The binding of C3b to phagocytic cell receptors improves pathogen adhesion to these cells, enabling pathogen engulfment in a phagosome.
Purposes in the Immune Response
- Efficiency boost: Complement-mediated opsonization improves phagocytosis efficiency, ensuring quick and effective pathogen clearance.
- Clearance Facilitation: It aids in the elimination of immunological complexes and apoptotic cells, hence contributing to immune system homeostasis.
Overall Impact in Immune Defense
Complement-mediated opsonization is an important mechanism by which the immune system targets and destroys pathogens, thereby maintaining homeostasis and protecting the host from infections. Its numerous contributions make it an essential component of the body’s defense against microbial attacks.
Opsonins and its types
Opsonins are substances that aid the immune system by promoting the process of phagocytosis, in which pathogens are consumed and eliminated by phagocytic cells. These compounds improve pathogen identification and binding to phagocytes, resulting in an effective immune response.
Types of opsonins
Antibodies
- Immunoglobulin G (IgG): IgG antibodies are adaptable opsonins that recognize and bind to a wide range of pathogens, designating them for phagocytosis. Their Fc (constant) region binds to Fc receptors on phagocytic cells, allowing them to be engulfed.
- Immunoglobulin M (IgM): Immunoglobulin M (IgM): IgM antibodies, particularly those in pentameric form, can act as opsonins. They have many antigen-binding sites, which improves their ability to bind pathogens and aid in phagocytosis.
Complement Proteins
- C3b: A pivotal opsonin that is produced throughout the complement cascade. It covalently binds to the surface of pathogens and foreign particles, improving phagocyte identification. C3b’s interaction with complement receptors on phagocytic cells promotes engulfment.
Collectins
- MBL (Mannose-binding Lectin): MBL is a soluble pattern recognition molecule that functions as an opsonin by attaching to particular sugar residues on pathogen surfaces. This interaction aids phagocyte detection and clearance of opsonized particles.
Fibronectin
- Fibronectin: This glycoprotein, by attaching to bacterial surfaces, can behave as an opsonin. Fibronectin improves phagocytosis efficiency by enhancing pathogen adhesion to phagocytic cells.
- C-Reactive Protein (CRP):
- CRP is an acute-phase protein that can function as an opsonin. It recognizes and binds to phosphocholine moieties on microbial surfaces. This binding improves phagocyte clearance of opsonized microorganisms.
- Serum Amyloid P Component (SAP):
- SAP (Serum Amyloid P Component) is another opsonin that interacts with pathogens and improves phagocytic cell identification. It modulates the immune response and promotes the clearance of opsonized particles.
Surfactant Proteins
- Surfactant Proteins (SP-A and SP-D): Surfactant proteins are opsonins found in lung surfactants. They aid in infection clearance from the respiratory tract by improving identification and phagocytosis.
Understanding the various activities of these opsonins sheds light on the intricate mechanisms used by the immune system to recognize and remove a wide range of infections and foreign particles.
Disorders Related to Opsonization
Immunodeficiencies and Impaired Phagocytosis
Background
Immunodeficiencies are diseases that cause the immune system to be impaired or compromised. Deficits in the generation or function of essential opsonins can result in decreased phagocytosis, a vital mechanism for pathogen elimination.
Implications
- Reduced Clearance: Phagocytic cells may struggle to recognize and engulf pathogens without efficient opsonization.
- Increased susceptibility: Individuals with opsonin-related immunodeficiencies are more susceptible to recurring infections.
Example:
- C3B deficiency: Lack of functioning C3b, a major complement opsonin, can result in poor opsonization and increased susceptibility to bacterial infections.
Autoimmune Disorders
- Systemic Lupus Erythematosus (SLE): SLE is an autoimmune illness in which the immune system hits healthy tissues by mistake. This can result in the development of immunological complexes that activate the complement system in some situations. Complement system dysregulation can impair opsonization and contribute to the immune system’s attack on self-tissues.
Chronic Granulomatous Disease (CGD)
- CGD is a hereditary condition that impairs phagocytes’ ability to create reactive oxygen species, particularly neutrophils. This dysfunction in the respiratory burst process can diminish the efficacy of phagocytosis, including opsonization.
References and Sources:
- Tortora, G. J., Funke, B. R., & Case, C. L. (2021). Microbiology: An introduction. Pearson Education Limited..
- Cappuccino J.G. and Sherman N. 2008. Microbiology: A Laboratory Manual, 8th ed. Pearson Benjamin Cummings, San Francisco, CA, USA.
- https://www.sciencedirect.com/topics/medicine-and-dentistry/opsonization
- Parija S.C., (2009), Textbook of Microbiology and Immunology, 2nd edition, Elsevier, a division of Reed Elsevier India Private Limited, pg. 94-115